FAQs
How should I prepare for my appointment?
It is essential that you have a valid referral from your referring doctor, along with information regarding any previous neurological investigations that you may have already had. Please see the ‘Preparing for Your Appointment’ tab for further information.
How much will the appointment cost?
Costs vary according to the consultation type (initial or follow up), consultation complexity (one main issue vs. two or more issues), and procedure type (EEG, NCS/EMG/repetitive nerve stimulation with procedures of varying lengths and complexities, and Botulinum toxin and other injections of varying procedure lengths and complexities), so both the Medicare rebate and the gap incurred by the patient will vary according to these factors. When you book your appointment with our secretarial staff, they should inform you of the cost based on the above factors before your appointment (and please specifically ask about these if they are not stated to you). A partial concession is offered for patients who are health care card holders or pension card holders.
Will there be any resultant driving restrictions?
This is by far the least pleasant although sometimes unavoidable aspect of working as a neurologist; there are certain neurological conditions (in particular seizures/epilepsy, functional neurological disorder mimicking seizures/epilepsy, strokes/transient ischaemic attacks/TIAs, dementias, visual problems, and significant upper or lower limb weakness or incoordination) which do often carry associated driving restrictions. The length of the restriction is relative to the particular condition and whether the licence is a private or a commercial licence, and is applied according to somewhat complex published guidelines (Austroads Assessing Fitness to Drive: https://austroads.gov.au/publications/assessing-fitness-to-drive/ap-g56). Restrictions also apply to boating and aviation licenses. Please note that this is a mandatory legal requirement that the neurologist and patient are both legally required to adhere to. Whilst understanding the marked practical challenges introduced by driving restrictions, particularly in regional Australia, these restrictions are designed and implemented by the government for the safety of both the patient and other members of the public, to avoid serious physical injuries or deaths. Please also note that these restrictions apply at the time of diagnosis (irrespective of whether the diagnosing doctor is a neurologist or otherwise).
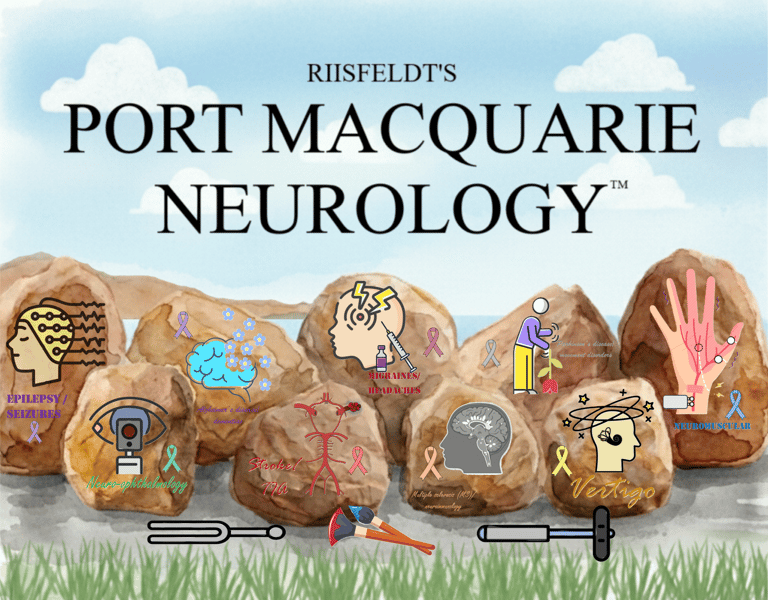
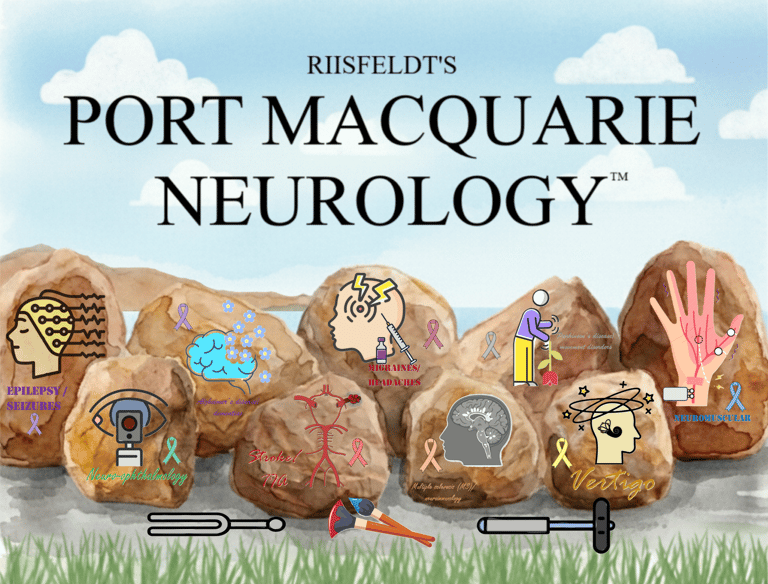
Can you explain your logo?
We thought you’d never ask! Our logo was designed personally and is a stylistic recreation of the Port Macquarie Breakwall Coastal Walk with its iconic painted rocks, with a beautiful view across to Pelican Point of North Shore. There are nine rocks, each with a carefully designed representation of the various branches of clinical neurology, consisting of altered versions of open-source logos found online. Moving from left to right, these are:
1. Epilepsy and seizures, with a head in profile undergoing an EEG, with the EEG leads then becoming the digitalised electrographic signals that we read, demonstrating sharp waves which can sometimes be seen in epilepsy.
2. Neuro-ophthalmology, with an eye undergoing fundoscopic evaluation with an ophthalmoscope, with the red retina on view.
3. Alzheimer’s disease and dementia, with a brain in profile, although with a degree of breakdown posteriorly to represent the posterior-predominant atrophy seen in Alzheimer’s disease. Many other logos used puzzle pieces or leaves to represent this process, with those pieces or leaves representing neurons (brain cells) floating away, but these have been replaced with forget-me-not flowers, the international floral symbol for Alzheimer’s disease and dementias.
4. Stroke/transient ischaemia attack (TIA), demonstrating a Circle of Willis, the loop of arteries which supply oxygenated blood from the heart to the brain. A thrombus has been added to the left middle cerebral artery (MCA), consistent with a left (dominant hemisphere) MCA ischaemic stroke.
5. Migraine and headaches, with a head in profile suffering from a unilateral headache, being treated with Botulinum toxin injections.
6. Multiple sclerosis (MS) and neuroimmunology, represented by a head in profile, which was initially an MRI in sagittal section fed through an artificial intelligence (AI) engine to make this look like a styled logo, followed my insertion of typical demyelinating white matter lesions of multiple sclerosis in the periventricular/callosal region (resulting in the classical ‘Dawson’s fingers’), along with some more subtle juxtacortical lesions, infratentorial lesions (in the cerebellum and brainstem), and spinal cord lesions, the four radiological areas of white matter lesions typical for multiple sclerosis.
7. Parkinson’s disease and movement disorders, demonstrating a patient in profile with a typical stooped posture and upper limb tremor seen in Parkinson’s disease. The walking stick has been replaced with a red tulip being used for the same purpose, the international floral symbol for Parkinson’s disease.
8. Vertigo and neuro-otology, demonstrating a dizzy head in profile. The semicircular canals have been added to the ear, and additionally some dislodged otoliths have been added to the posterior canal, which is the most common form of benign paroxysmal positional vertigo (BPPV).
9. Neuromuscular diseases, represented here by a hand with sensory disturbance affecting the palmar aspect of the 1st, 2nd, 3rd and first half of the 4th digit in the distribution of the median nerve, commonly caused by carpal tunnel syndrome from entrapment and compression of the median nerve at the wrist. An NCS setup has been added, with the median nerve being stimulated at the wrist, the active recording electrode being placed on the belly of the abductor pollicis brevis (APB) muscle, and the reference recording electrode placed on distal tendon of that muscle, and the ground electrode on the dorsal surface of the hand, the standard arrangement for a motor NCS for the median nerve.
The writing at the bottom of each rock is in different text, representing the wonderful variety of the Breakwall art, and the text and accompanying ribbon for each rock is in the colour of the ribbon of the international awareness day for the respective conditions (e.g. purple for epilepsy and seizures). Paint brushes are included to highlight that the logos are painted on each rock, along with symbolising the ‘art of medicine’, not to be forgotten and always being balanced against the ‘science of medicine’. Finally, on the walking path, a tendon hammer and tuning fork lie at the base of the rocks, representing the clinical method (especially the clinical examination in neurology, both motor and sensory aspects) as the foundation or ‘roots’ of the diagnostic process, with grass and their literal roots lying adjacent to them on the other side of the path. You can probably tell that more than a little thought went into this overall design so we really hope that you appreciate it!